I find it ridiculous that patients are sent home from surgery with instructions about pooping and bathing, but nothing about the potential emotional complications of surgery.
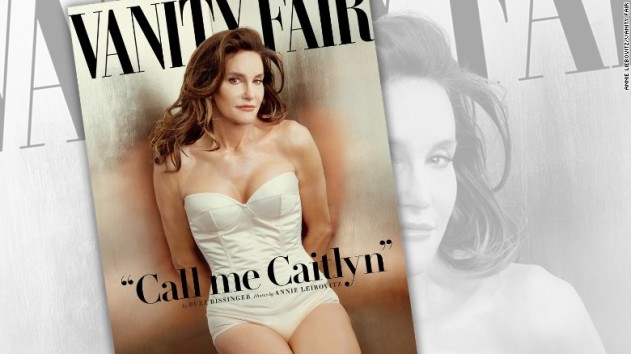
Just when you thought Caitlyn Jenner couldn’t be a better role model or teach us more, she slipped an important side note into her Vanity Fair debut.
In the interview, Jenner talked about an emotional crisis she experienced the day after she had undergone a facial surgery that took 10 hours and was significantly more traumatic than she had expected. She had a full-blown panic attack and found herself thinking: “What did I just do? What did I just do to myself?”
Fortunately, Jenner had support from people familiar with post-surgical emotional complications: “A counselor from the Los Angeles Gender Center came to the house so Jenner could talk to a professional, and assured her that such reactions were often induced by pain medication, and that second-guessing was human and temporary.”
I am very glad that Caitlyn had access to good post-surgical counseling. I cannot emphasize enough how important it is for people undergoing surgery to have at least one person on their team who understands post-surgical depression and the other emotional problems that surgery can precipitate.
But why wasn’t she prepared for this to happen? Why did no one on her team warn her about the mental health complications that often accompany a painful surgery? What she experienced was entirely predictable given how long the surgery was and how painful it likely was. I believe that Caitlyn would have experienced less distress if she had been educated about what happens to many people emotionally following long and invasive procedures.
I find it ridiculous that patients are sent home from surgery with instructions about pooping and bathing, but nothing about the potential emotional complications of surgery. If nothing else, the instructions should warn people that certain kinds of pain medications can cause you to feel overwhelming negative emotions.
I know those negatives emotions well—I am a surgery veteran. When I was 25, I was in a serious accident that left me with orthopedic issues that have required several surgeries. Along the way, I have learned a lot about how to cope with the aftermath of surgery.
Two years ago, I wrote an article on the subject that people are still reading. I still get messages from people who had similar experiences. From them, I have learned that post-surgical depression is extremely common. I have also learned that there is a huge gap in medical care around post-surgical emotional and mental health complications.
Doctors have long been aware that many patients experience some form of post-surgical depression during the six months following an invasive procedure. But many physicians believe that being depressed after surgery is “understandable” and “unworthy of diagnosis or treatment.” They believe that because most patients emerge from depression after about six months, post-surgical depression is either benign or even helpful since it keeps people inactive.
Most people do not know that post-operative depression is a common complication of surgery. Information on the subject is sadly scarce.
Caitlyn’s experience makes two things very clear. The first is that the emotions people experience after surgery often have no basis in reality. Caitlyn unquestioningly wanted to transition in the way that she did and had sacrificed a great deal to do so. But pain and drugs lie to us. Like Caitlyn, I have had moments after surgery where I ask myself “What have I done?” even when the surgery was necessary to keep me ambulatory.
The second thing that Caitlyn’s story shows is that knowledge brings relief. She seems to have taken great comfort from knowing what was going on with her.
It’s important to point out that Caitlyn’s crisis occurred at a predictable time relative to her surgery. It was the second day, when pain often spikes. People tend to think that the worst of the pain is over by then, and so they are surprised and panicked when hit by the post-surgical pain-spike. It can be a very frightening experience.
After my most recent surgery, a total knee replacement that was complicated by the extensive nature of the precipitating injury, I was given both Vicodin and Dilaudid. While the combination was very good at combating the extreme pain I was experiencing, the Dilaudid caused me to have very strong waves of negative emotions including suicidal ideations.
I had no idea that what I was experiencing was a known side effect of the Dilaudid. Luckily, my psychiatrist had personally experienced a similar reaction to the drug. As she put it, “The sanest people can fall apart on that stuff.” We talked about changing my medication, but since it was so good at controlling the pain, we decided against it. Just knowing what was causing me to have the tsunami of negative emotions allowed me to observe them without being swept away by them.
Information makes all the difference.
We must make sure that every patient who is about to have surgery knows that the aftermath could be some sort of emotional crises or depressive event. We must make sure that family members and other people who provide post-surgical support are aware that this can happen. And we must support research into which medications have the fewest mental health side effects.
Lynn Beisner writes about family, social justice issues, and the craziness of daily life. Her work can be found on Role Reboot, Alternet, and on her blog: Two Parts Smart-Ass; One Part Wisdom. You can find her on Facebook and Twitter.
Related Links: